You could ask a similar question regarding your car:
“what objective evidence makes you confident that your car can drive you safely to your destination?”
The answer is three-fold (see post 1/3 for the first evidence).
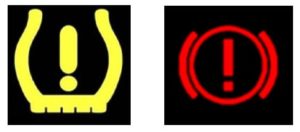
Second objective evidence: unless your car is a very old one, you know that you can rely on its electronic system to activate a visual alarm and a sound as soon as it detects an event that can represent a risk. The visual sign may be intuitive enough to easily and quickly decide which action should be taken to correct the issue. Alternatively, you could also refer to the car leaflet where the action to be taken is explained next to each control panel warning light. The alarm resumes as soon as the issue is corrected.
In a similar manner, the second objective evidence that your clinical study data integrity is under good control may come from key data quality indicators which can be produced during the course of the study.
These should be monitored appropriately and raise alerts as soon as data quality signals potentially critical to the study are detected. Corresponding action plans should be defined and documented, as well as followed through up to resolution of the issue.
As in the case of your car, you should not receive too many of these alerts, since you should not be diverted from your study execution plan unless an event of critical nature happens and needs to be raised to you.
Key data quality indicators should therefore be set to rapidly detect only the few issues having a potentially high impact, such as:
=> Data integrity or quality issues leading to potential risks on the safety, physical or mental integrity of the subjects of the trial, e.g.:
- an electronic algorithm that computes a score used to assess an inclusion or exclusion criteria does not provide an accurate result, leading to a jeopardised subject population
- under reporting of adverse events by a site
- under or over reporting of serious adverse events by a site
=> Data integrity or quality issues leading to a potential risk for the scientific value of the trial, e.g.:
- fraud or data tampering by a recruiting site
- presence in a data transfer of data that un-blinds the intervention assigned to study subjects (for a blind study protocol)
- high amount of missing records for the primary efficacy endpoint assessment
- error in the setup of the central randomisation system leading to a randomisation bias
- wrong programming of a data transformation step leading to the loss of critical data records
- transfer of protocol deviations records not properly tested or quality controlled leading to an incorrect allocation of subjects to the analysis populations
You may want to be alerted, if not real-time, with an acceptable delay, if any of the above issues arise, in order to ensure a proper root cause analysis is quickly conducted, corrective actions implemented, and, if possible, preventive actions taken to avoid re-occurrence of the same issue.
Key data quality indicators should better be defined and the detection tools selected and setup before the study starts. As part of its methodology, « alcoam by design » uses its template « key data quality control panel specification table », and tailors it to your study critical needs.
Obviously, you would not only rely on your car control panel warning lights to be confident on its ability to drive you safely, especially if you have a long journey ahead. More visual inspections and periodic controls are needed in addition, to prevent or correct issues that are not monitored by the electronic sensors system.
For your study, you may need reassurance that all the necessary periodic controls regarding the compliance to data quality and integrity requisites (do you remember? – ALCOA-CCEA) are properly and timely executed, so your study costs and delays remain under good control.
We will look at the third type of objective evidence of integrity you could seek for your clinical study data in the post 3/3.
Isabelle Abousahl
President at alcoam by design SAS
